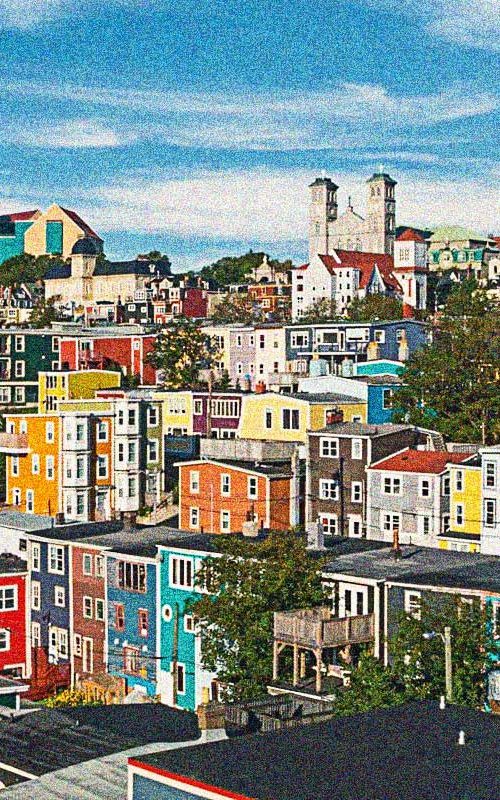
CCLA Granted Leave to Challenge Arbitrary Travel Restrictions Before the SCC
Arbitrary travel restrictions infringe on the mobility rights of Canadians. CCLA’s challenge of Newfoundland government’s Bill 38 will continue before the SCC, so that Canadians have clear, predictable, and stable…